

Thus, for a certain percentage of IMN-positive/axillary node negative patients with small tumors, the underestimation of the nodal status could lead to a dispense of adjuvant therapy, resulting in a decrease of survival.įor no one would claim the indication for a systematic parasternal dissection in small, axillary node negative tumors, the problem of the IMN-status remained unresolved up to now. The expected rate of IMN-positivity in axillary negative patients is about 17–20% and the risk of recurrence or death at 10 years is twofold greater, if the patients receive no adjuvant therapy.
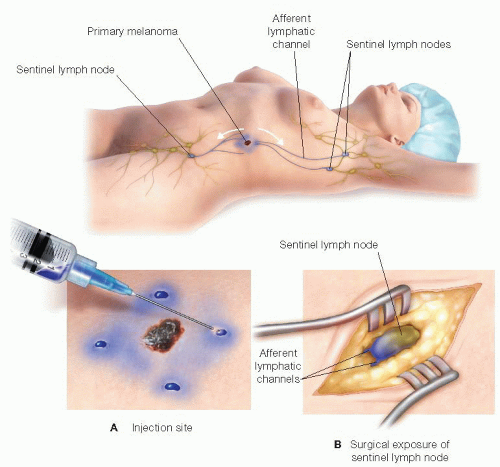
Involvement of IMN, however, is strongly related to axillary node involvement and its prognostic significance is the second most important factor for survival after axillary node status. It has been shown, that extended radical mastectomy with dissection of the internal mammary nodes did not improve longterm survival in large groups of patients with tumors of all sizes. Nevertheless, some work groups have recently begun to evaluate a combination of the two methods. In breast cancer “the passthrough” effect in the draining lymph nodes is obviously not as pronounced as it is in melanoma, therefore the phenomenon of second-tier lymph node in breast cancer patients does not seem to require an additional blue dye staining, if the radionuclid method has been successful. Whereas some study groups in the USA (Giuliano et al.) still use the blue dye technique, the radionuclid method, as described above, is the method of choice for most of the study groups in Europe. The sentinel node concept is currently in evaluation to avoid costs and morbidity for this group of patients and to select very specifically the node positive patients for axillary dissection.Īfter having gained experience with the method, a sentinel node can be identified in 93–98% of the clinically node negative patients with early breast cancer (tumor diameter 0,5–3 cm) and predict the nodal status correctly in 95–99%. Equally, the rate of nodal negative axillary dissections increased to 70–80% in clinically node negative patients with a tumor diameter between 1 and 3 cm. With the ongoing introduction of tumor prevention and the increasing sensitivity of imaging procedures, the tumor size at the time of diagnosis has decreased dramatically in the last years. The largest experience with the sentinel node concept exists for patients with melanoma and breast cancer, where the method is clinically applicated and has already reached influence on therapeutic strategies for certain patient subgroups. For dynamic lymph flow studies, requiring a high transport velocity, pure albumine solutions are used, with a particle size of 3–5 nm. They require a longer time period between injection and surgery but offer the possibility of several preoperative y-ca-mera pictures and a constant activity during the operative procedure. They undergo phagocytosis by macrophages, show a long storage time in the lymph nodes and the time for the transport from the injection site to the lymph node is longer as for sulfur colloids. In Germany and Europe widely used are heterogenous solutions of albumine derivates (Nanocoll) with a particle size ranging from 80–200 nm. There are several substances, which had been used as tracer colloids: In the USA mostly used is Tc 99m-sulfur colloid with an average particle size of about 10 to 50 nm showing a relative fast movement from the tumor to the lymph nodes and a rather fast extraction out of the lymph node along with the efferent flow due to the capability to pass through the vascular epithelial cell gaps requiring an injection time of about 2 hours before surgery. The size of the colloid shows an inverse correlation to the velocity of its transport along the lymphatic channels and a direct correlation to the duration of the storage in a lymph node. It is important to know, that the size of the tracer colloid is crucial for the quality of the transport with the lymph flow and how long it is stored in the lymph nodes.


 0 kommentar(er)
0 kommentar(er)
